How tiny? They’re measured in nanometers, which is one-billionth of a meter. Like the width of a marble compared to the width of the Earth.
By going that small, Koenigsmann and his students have innovated in the areas of biomedical sensors and sustainable energy technology. Now his lab has a new project: scrubbing the air clean of viruses like the one that causes COVID-19.
Preventing Cases of COVID-19
Koenigsmann sees a way to improve on a type of indoor air purifier—activated by ultraviolet light—that destroys particles of coronavirus and other viruses but can also create tiny amounts of toxic byproducts under certain conditions.
Such devices have been around for decades, and were used in hospitals to remove tuberculosis from the air, “so it’s a proven technology,” said Koenigsmann, an associate professor in the chemistry department. “It’s just [that] as it becomes scaled up and more broadly used, and in environments where the air is not tested as regularly, that’s where you can run into problems.”
He and his team are working on new technology that could break down viruses without releasing toxins, which could lead to new types of purifiers that destroy viruses on a greater scale. On a recent summer day, in a lab at the Rose Hill campus, they were getting ready to run experiments using ductwork and a filter containing new types of nanoparticles.
The lab also includes a high-temperature reaction chamber and other tech for making the nanoparticles themselves—indispensable because they’re so small.
Surface Appeal
Koenigsmann, an associate professor in the chemistry department, has long been fascinated with “being able to tune fundamental physical properties” of a substance by changing its size or other aspects.
Break a substance down into smaller units, he explains, and suddenly it’s a lot better at reacting with things, since a lot of small particles will have more total surface area than a few large ones.
How much more? If you’re turning something into nanoparticles, one square meter per gram could become hundreds of square meters per gram. “For the same amount of mass, you gain a tremendous amount of surface area,” he said.
And more surface area means more reactions. For instance, a battery made from nanoparticles offers vastly more internal surface area for conducting an electric current. And air purifiers operating on the same principle offer more surface area for reacting with viruses and churning them up.
Filtering Coronavirus
In some of today’s air purifiers, Koenigsmann said, titanium dioxide chews up a virus particle in a chemical reaction that yields carbon dioxide when it runs its course—but formaldehyde, carbon monoxide, or other toxins when it doesn’t.

To address this problem, Koenigsmann and his team are working on new types of nanomaterials that, because of their size and composition, will fully break down virus particles, giving off only carbon dioxide and opening the door to purifiers that are safe to use more widely.
His undergraduate students contribute a lot to the project—“They’ll tell you things that you wouldn’t have thought of yourself,” he said. “I’m actually learning as my students learn.”
The uses for nanotech seem endless, Koenigsmann said. “The ability to tune things like conductivity, color, catalytic activity, just by making the same material one shape or one size versus another [has] so many possible applications,” he said.
]]>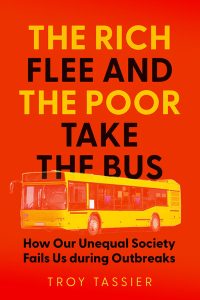
During the COVID pandemic, a story in the New York Times caught the eye of economics professor Troy Tassier, Ph.D. Using anonymous cell phone data, researchers showed that nearly 50% of residents in New York City’s wealthiest communities had left the city.
Those in poorer communities stayed for the most part, working at in-person jobs and commuting along their normal bus and subway routes. As a result, Tassier said, in the first year of the pandemic, the rate of mortality in some of the hardest hit, poorer neighborhoods was five to six times higher than it was in affluent areas in New York City.
It inspired Tassier to produce research on herd immunity and other infection-related data. In February, he published The Rich Flee and the Poor Take the Bus: How Our Unequal Society Fails Us during Outbreaks (Johns Hopkins Press, 2024), which investigates how social inequality affects epidemic outbreaks.
The book examines pandemics from the past, from the Bubonic plague that devastated Hong Kong in the 19th century to the influenza pandemic that ravaged New York City in 1918. Why was it so important to highlight this history?
At the beginning of the pandemic, there was this narrative that this was a great equalizer, but I knew it wasn’t going to be true, just from past pandemics. In New York City in the 19th century, poor people were blamed for the pandemics because they were afflicted more than wealthy people. But it wasn’t their fault; it was the conditions that they were living in. During COVID-19, we were experiencing some of the same things.
Were you surprised by anything you encountered while doing your research?
The biggest surprise was just how similar past epidemics were to what happened in 2020, down to things like fights over masks. There’s a story from 1918 about a fight between a health inspector and a person standing on the street corner who was arguing with people, telling them they were fools to be wearing masks. They ended up in an altercation, and a couple of people were shot.
I have a cousin who lives in the South who was doing curbside pickup at a store in 2021, and she was accosted by two guys who tried to rip the mask off her face.
A major point of the book is that we should treat medicine as a social science. Do you think the pandemic made that clear to people?
No, and that’s one of my biggest disappointments. You still hear refrains coming from both the left and the right that public health needs to step away from proselytizing and just “follow the science,” but part of that science is how people are reacting to policies and to each other.
Something I’ve been grappling with is, last month the CDC eliminated the five-day isolation period following a positive infection. Now, these isolation periods are regressive because they harm working people who don’t have paid sick leave or might not be able to afford childcare if their child has to stay home to be isolated.
But the CDC shouldn’t be saying there’s a problem with the regressive nature of this five-day isolation; therefore, we need to get rid of the isolation period. What they should be saying is we have these problems in society, and we need to work to get rid of this inequality.
It’s not just as simple as people raising themselves up by the bootstraps.
]]>But was that air pollution actually causing those symptoms?
In a new study published this month, Marc Conte, Ph.D., professor of economics at Fordham, says no.
“There’s no question that air pollution is a public health threat, but measuring the impacts of air pollution on humans, whether it’s cognitive ability, physical health, or mental health, is pretty challenging,” said Conte.
Correlation vs. Cause
The challenge, he said, is overcoming the temptation to put more weight behind observational studies than they deserve. A researcher might collect data and determine that a large number of people with dementia have bad teeth. But that doesn’t necessarily mean that bad teeth cause dementia.
“The public health researchers who are conducting this work know that they’re studying correlations, but when the media reports on these studies, the layperson who consumes that information might not necessarily know that it’s a correlation and not causal,” he said.
For the study, “Observational studies generate misleading results about the health effects of air pollution: Evidence from chronic air pollution and COVID-19 outcomes,” which was published in the journal PLOS ONE, Conte and his research partners paired data from two different sources that were collected between March and September 2020.
The first source was health data gathered from U.S. Census tracts in New York City, whose geographic centers are less than 500 meters from a highway. That narrowed the number of tracts studied down to about 800 out of a total of 2,168 in New York City. The researchers then compared that to data collected from the New York City Community Air Survey, a network of 100 air quality monitors maintained around the five boroughs.
That extensive network, which augments a much smaller number of monitors in New York City maintained by the federal government, allowed researchers to compare communities that are downwind from highways with those that are upwind. If poor air quality were responsible for more severe COVID symptoms, communities downwind would be expected to fare worse than their upwind neighbors.
Findings
Conte said that across the 800 census tracts, there was no statistically significant difference between those who were downwind and thus had poorer air quality and those who were upwind and therefore had better air quality. Other factors, such as income differences, access to health care, and the ability to work remotely during the pandemic, are more likely culprits for severe symptoms, he said.
In addition, many residents in these areas were unable to leave New York City at the height of the pandemic, either because they lacked the means to do so, or their jobs required that they work in person. The inability to engage in this kind of “defensive behavior,” resulted in higher exposure to those infected with the virus.
“That fact suggests this issue of environmental justice extends beyond the fact that certain communities are located near more pollution sources,” he said.
“It’s actually a more systemic problem that lower-income people are employed in positions that could not accommodate remote work, with many designated ‘frontline’ workers,” he said, or simply didn’t have the resources to leave the city.
None of this means that researchers should cease conducting observational studies, especially during health emergencies like the pandemic, Conte said. Rather, he hopes the study will further elevate the notion that “correlation does not equal causation” in the public consciousness.
More Data = Better Outcomes
A second takeaway from the study is the importance of maintaining a large network of air quality monitors, which together are able to generate finely detailed data. In fact, Conte’s team also conducted a second experiment on the same topic using only data collected by the seven monitors maintained around New York City by the Environmental Protection Agency, without any input from the New York City Community Air Survey.
The results were much closer to the observational studies that had been done and might have led readers to believe that air pollution and severe COVID symptoms are explicitly linked to each other.
“As we think about things like wildfires and other sources of air pollution, these problems are becoming more and more intense,” said Conte.
“For us to be able to take measures that can reduce the public health outcomes and the threats to public health, we need to have more information. We need to invest more.”
]]>

 What’s the best way to communicate health-related warnings to young people, who are more prone to taking risks? A recent study by Fordham students and faculty offers some possible answers—and they’re closely related to Fordham’s Jesuit values.
What’s the best way to communicate health-related warnings to young people, who are more prone to taking risks? A recent study by Fordham students and faculty offers some possible answers—and they’re closely related to Fordham’s Jesuit values.
The idea for the study emerged in fall 2020. Fordham had reopened its campuses after its University-wide pivot to virtual instruction the previous March, and was requiring masks as well as other precautions to contain the coronavirus. Universities everywhere were doing similar things, hoping to avoid COVID-19 spikes that would force them to once again shift to completely remote education.
When this shift didn’t need to happen that fall at Fordham, students sighed with relief. And a student-faculty cohort in the psychology department grew curious.
“As a group that studies health behaviors especially among young adults, we were fascinated by this,” said Rachel Annunziato, Ph.D., associate dean for strategic initiatives and professor of psychology at Fordham College at Rose Hill. “I thought, ‘There’s probably something special about Fordham students that’s contributing.’”
She and her student researchers in the Pediatric Psychology and Health Behaviors lab prepared a survey that was completed by 92 students before the planned closure after Thanksgiving break. It asked about their level of compliance with masking and other measures to contain the coronavirus. It also measured motivators including empathy and concern for the collective good, which dovetail with the Jesuit identity of the University.
 Maura Mast, Ph.D., dean of Fordham College at Rose Hill, was a senior author of the study, titled “Students for others: Correlates of adherence to COVID-19 guidelines.” The title reflects a key precept of Jesuit education that is constantly reinforced, noted one of the student co-authors, Kristina Stevanovic, FCRH ’22.
Maura Mast, Ph.D., dean of Fordham College at Rose Hill, was a senior author of the study, titled “Students for others: Correlates of adherence to COVID-19 guidelines.” The title reflects a key precept of Jesuit education that is constantly reinforced, noted one of the student co-authors, Kristina Stevanovic, FCRH ’22.
“From the second you arrive on campus, [Joseph M. McShane, S.J., now president emeritus of Fordham] talked about being men and women for others, and any Fordham event you attend where they’re talking about Jesuit values, it’s men and women for others,” she said. “Maybe it just is the fact that we hear it over and over again.”
Promoting Health Awareness in the Young
The study, published in July in the Journal of American College Health, is one of many to grapple with the question of how to get adolescents and young adults to take health precautions seriously, even though they’re more likely to take risks and may find it hard to make a behavior change if their peers aren’t doing the same thing.
A lot of the work in Annunziato’s lab centers on young people’s adherence to medication regimens after receiving liver transplants, so focusing on coronavirus precautions “felt like a natural shift,” said another coauthor, Rebecca Tutino, a doctoral student in clinical psychology at Fordham. She also noted that the topic was close to home for the student researchers.
“We [were]all students ourselves going through the same lived experience as everyone else who took part in this study.”
Students’ health behaviors weighed heavily on leaders as universities everywhere grappled with how to approach the fall 2020 semester, the study says. Out of 3,000 institutions surveyed by the Chronicle of Higher Education about their reopening modes, the study notes, 34% offered courses primarily online, 23% were primarily in-person, and 21% were in hybrid mode. Only 10% were fully online.
Fordham took a blended approach—after shifting to remote education in March 2020 following the pandemic’s outbreak, the University offered hybrid courses in fall 2020 and gave students the option of taking all their classes online. Residence halls opened, and masks, social distancing, and other precautions were required. If COVID cases had totaled 5% of the on-campus population, Fordham would have had to return to fully remote learning for two weeks, per New York state policy.
Rates stayed low and stable through Thanksgiving break, after which Fordham pivoted to remote learning for the remnant of the semester, as it had planned to do since the prior summer. The low COVID rates were a nice surprise, Tutino said—“We were like, what is going on here? What is it about our student body that is allowing for this to happen?”
Their study offers some insight.
Survey Results
Students completed a web-based Qualtrics survey during the month leading up to Thanksgiving break in 2020. The results showed students were largely following the rules—for instance, more than 90% were washing their hands and wearing masks both inside and outside, either all or most of the time. More than 90% were mostly abiding by travel restrictions, and nearly 70% were practicing social distancing all or most of the time.
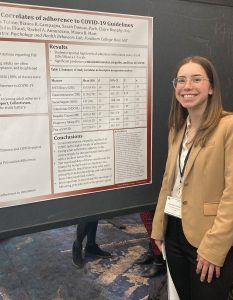
Their reasons for complying were the key finding, Annunziato said. A less-prominent reason was social support, or feeling like one’s peers support your actions—usually a strong predictor of health-related behaviors. Also less prominent was self-efficacy, or one’s sense of personal control over an outcome or circumstance.
Instead, students’ behaviors were more driven by empathy, fear of COVID, taking others’ perspective, and a sense of collective benefit. Stevanovic noted the interrelations between these reasons—“If you’re able to put yourself in somebody else’s shoes, I think you’re a little bit more likely, then, to have a collectivist attitude, and espouse greater empathy,” she said. “I can just clearly see how those constructs end up relating and being correlated to one another.”
Tutino said the findings line up with what she saw among students in her program—respecting other people’s boundaries, taking care to sit far enough apart in class, or perhaps opening windows to make everyone feel comfortable and safe, she said.
The study notes some possible limitations: for instance, most respondents were women, and they held more liberal political views. And they had chosen to attend a Jesuit university that embraces certain values.
Future Directions
But the study still offers useful insights, Annunziato said. “In my field of pediatric psychology, I’ve talked to a lot of folks who are intrigued by this,” she said. “We really struggle in terms of developing interventions that are meant to cultivate or bolster health behaviors. I think there’s excitement that the Fordham experience has helped to maybe fill in some missing pieces when it comes to motivators of young adults.”
The findings show that empathy and collectivism could have bearing on other health behaviors such as underage drinking or getting vaccinated, the study says.
Stevanovic presented the research in March 2022 at the Eastern Psychological Association Conference in New York City, where she saw a lot of research projects related to COVID. Because of this experience, “I think I really just want to study health behaviors, ultimately, and population health,” said Stevanovic, who is now a clinical research coordinator in psychiatry and behavioral sciences at Memorial Sloan Kettering Cancer Center.
Tutino noted that “we got so many responses right away” after posting the study’s questionnaire.
“To see such a high response rate and to have people sending the links to each other and sharing it without us even having to ask, that was really wonderful,” she said. “I feel like all of us were thinking, ‘Why aren’t we doing this more?’ This is a population that’s happy to help us with our research, and we can really learn so much from them.”
]]>I am writing to remind you that all University faculty, students, and staff must be up-to-date as defined by the CDC as of Tuesday, November 1, 2022—meaning individuals must receive the updated (bivalent) booster if it has been 2 months or longer since their last COVID-19 vaccine, or 90 days after recovering from a COVID-19 infection. The same standards apply to campus visitors, guest speakers, and visiting athletic teams.
Individuals may request medical or personal religious exemptions to the vaccine mandate: faculty and staff should email Human Resources at occ-health-medicine@fordham.
After the November 1 deadline, the University will be contacting any individuals who have neither provided the appropriate documentation demonstrating they are up-to-date with the vaccine, nor have received an exemption, to confirm their compliance. Individuals who continue to remain non-compliant will ultimately have their access to campus restricted.
Being up-to-date on the vaccine is particularly important because of an increase in COVID-19 infections in the UK and Europe, including the new BQ.1.1 subvariant. Public health officials believe that the infection spike in the UK and Europe presage a fall/winter wave of infections in the U.S.
Being a community that is up-to-date on vaccinations has allowed Fordham to operate largely without masking and social distancing requirements. There is an abundant body of evidence that boosters reduce the transmission of the virus. The pandemic’s lethality has been blunted because of widespread vaccination for COVID-19, but COVID-19 remains a public health threat which still has the capacity to shut down our campuses.
While being up-to-date on vaccinations is important for everyone, it is critical for people living in group settings such as University housing. The Fordham community is composed of people of all ages, and there are many faculty, staff, and students who are vulnerable for factors seen and unseen.
The University has the new updated bivalent vaccines in stock and will administer them free of charge. Individuals can walk in for vaccines at the times and locations listed on the Testing and Vaccine Resources Page. (The updated bivalent vaccines are also available in the New York City area.) Individuals who received their vaccinations off campus should upload proof of vaccination to VitalCheck by clicking on the link text “Has your vaccination status recently changed?” on the daily VitalCheck email/text message.
COVID-19 and flu vaccines both reduce illness, hospitalizations, and deaths. As flu season approaches and COVID-19 vaccine recommendations are updated, individuals should consider receiving both vaccinations at the same time if they are eligible and the timing is appropriate. The immune response and possible side effects are generally the same whether individuals receive one vaccine at a time or two, according to the CDC.
Employees with questions about Fordham’s COVID-19 policies should email vpforadministration@fordham.
As always, our policies and protocols are subject to change, based on conditions on and off campus, and any new federal, state, or local regulations.
Finally, please accept my profound thanks, and that of the University administration, to those of you who are staying up-to-date on your COVID-19 vaccinations. By doing so you are saving lives and helping to keep the members of the Fordham community healthy and safe. Your willingness to get vaccinated is cura personalis in action, and it is deeply appreciated.
Marco Valera
Vice President for Administration & COVID-19 Coordinator
Accordingly, the University updated its protocols, requiring faculty, students, staff, and guests to be fully up-to-date as defined by the CDC by Tuesday, November 1, 2022. Visitors must follow the same protocol. More information is available on the COVID-19 Vaccine Requirement webpage. This message was shared with all students, faculty, staff, and parents on September 27. The University had communicated the likelihood of this update in protocol to the University community and parents since April 2022 (see the communications history below).
Individuals may still request medical or personal religious exemptions to the vaccine mandate: students should contact University Health Services; faculty and staff should email Human Resources at [email protected].
COVID-19 remains a public health threat. To the extent that the pandemic’s lethality has been blunted, it is because of widespread vaccination for COVID-19. People are still getting sick, but the percentage of those who require hospitalization or who die is much lower—this, by itself, is reason enough to require everyone on campus to be vaccinated and boosted.
Unfortunately, COVID-19 still has the capacity to shut down our campuses. While being up-to-date on vaccinations is important for everyone, it is critical for people living in group settings such as University housing. The Fordham community is composed of people of all ages, and there are many faculty and staff (and some students) who are vulnerable because of their age and other factors.
Fordham already requires proof of immunizations for measles, mumps, rubella, and meningitis—and has done so for decades. Like those diseases, COVID-19 is a public health issue, and the relevant authority is the CDC. It recommends everyone stay up to date with COVID-19 vaccination, including all primary series doses and boosters for their age group.
We follow CDC guidelines because it has both access to the scientific literature and the expertise to interpret the data and make recommendations based upon it. The CDC bases its guidelines on the work of many researchers, virologists, and epidemiologists—a depth of experience and expertise beyond what can be expected from individual medical practitioners.
Vaccine manufacturers roll out new flu vaccines every year without clinical trials: likewise, the new COVID-19 vaccines, which protect against variants, is based upon established vaccines. It is rare in the history of vaccines to have so few people suffer side effects. The CDC’s vaccine safety page addresses the concerns of those who are hesitant to receive vaccines/boosters under several headings:
- Hundreds of Millions of People Have Safely Received a COVID-19 Vaccine
- Adverse Events (Serious Safety Problems) Are Rare
- The Benefits of Vaccination Outweigh the Risks
All of which can be found here: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/safety/safety-of-vaccines.html
As an institution that practices care for the whole person, we have to follow the lead of public health authorities.
Communications History
Prior to September Fordham students, faculty, staff, and parents received the following messages via email (which were also posted to the website and social media):
- July 27, 2022: As of September 1, students, faculty, and staff are required to be fully up-to-date, as defined by the U.S. Centers for Disease Control and Prevention (CDC).
- May 6, 2022, April 28, 2022, April 20, 2022, April 13, 2022, and April 1, 2022: Fordham Vaccine Mandate: The University will continue to require all on-campus students, faculty, and staff to be fully up-to-date† on vaccinations for the 2022-2023 academic year. It may be necessary to require a second booster shot for eligible individuals beginning in September 2022. †“Up-to-date” means the individual has received a full series of COVID-19 vaccines, and a booster shot, if eligible.
New students and their parents received email regarding the vaccine requirement on June 1, 2022: “Fordham University requires all students who are taking in-person classes, living in University housing, or entering the campus for any reason to be up to date with their COVID-19 Vaccines, which currently includes one booster dose.” and on the linked page: “It may be necessary to require a second booster shot for eligible individuals for the 2022-2023 academic year.” New students and their parents received similar messages on July 29, August 23, and August 29.
]]>
Dear Members of the Campus Community,
I am writing to give you an update on University COVID-19 protocols. I hope your fall semester is going well. I’m sure you are busy, so I will make this as brief as possible.
Vaccinations
According to the U.S. Centers for Disease Control and Prevention (CDC), individuals 12 and older are eligible for the updated (bivalent) booster that is effective against multiple COVID variants, and in order to be considered up to date with vaccines, they should receive the updated booster if it has been 2 months or longer since their last COVID-19 vaccine. Individuals under 18 can only receive the Pfizer updated booster. The updated Moderna booster is only available for those 18 and over. Being up-to-date on the vaccine is particularly important because it will be more effective against new variants of the virus, helping us to both keep our community safe, and to function with less disruption.
The University has the new updated vaccines in stock and will administer them free of charge. You can sign up for the vaccine on the Testing and Vaccine Resources Page. (The updated vaccines are also available in the New York City area.) Members of the campus community must receive the updated vaccine as soon as they are eligible—individuals who have tested positive for COVID-19 within 90 days will have the deadline for compliance adjusted accordingly.
All University faculty, students, and staff must be fully up-to-date as defined by the CDC as of Tuesday, November 1, 2022.
Individuals can upload proof of vaccination to VitalCheck by clicking on the link text “Has your vaccination status recently changed?” on the daily VitalCheck email/text message.
COVID-19 and flu vaccines both reduce illness, hospitalizations, and deaths. As flu season approaches and COVID-19 vaccine recommendations are updated, individuals should consider receiving both vaccinations at the same time if they are eligible and the timing is appropriate. The immune response and possible side effects are generally the same whether individuals receive one vaccine at a time or two, according to the CDC.
Reporting a Positive Test and Contact Tracing
The methods for reporting a positive COVID-19 test remain the same, but the University has changed its contact tracing and isolation procedures. Public Safety contact tracers will contact individuals with positive tests to determine the start date of their symptoms, and advise them of isolation and masking protocols available on the Isolation and Quarantine Procedures page.
Testing
Individuals may obtain a free PCR test on campus on Tuesdays and Thursdays from 9 a.m. to 3 p.m.
- Rose Hill Campus: First trailer in parking lot A.
- Lincoln Center Campus: Lowenstein Center, South Lounge.
For all contacts, regardless of vaccination status, quarantine is not necessarily required; however, if symptoms occur, individuals should immediately quarantine until a negative test confirms symptoms are not attributable to COVID-19
Faculty are not required to notify a full class about individuals in their classes who test positive. Should faculty choose to communicate with their classes, they should not identify the individual who tested positive.
Masking
New York state has relaxed its rules regarding masking on mass transit. Accordingly, masks are now suggested but not required on Ram Vans.
Employees with questions about Fordham’s COVID-19 policies should email vpforadministration@fordham.
As always, our policies and protocols are subject to change, based on conditions on and off campus, and any new federal, state, or local regulations. Thank you for your support and cooperation.
Marco Valera
Vice President for Administration & COVID-19 Coordinator
But if health authorities want to convince parents to vaccinate children in this age group against COVID, they’re going to have to acknowledge that this isn’t 2020 anymore, said Celia Fisher, Ph.D.
“One of the things we found was that the resistant and unsure parents are saying, ‘Look, the vaccine doesn’t work, because people who’ve been vaccinated are getting COVID. So why should I give it to my child?” said Fisher, the Marie Ward Doty University Chair in Ethics and director of Fordham’s Center for Ethics Education.
Just as the center did last fall, when the FDA authorized the use of vaccines for 5- to 11-year-olds, Fisher, who collaborated with Fordham graduate students Elise Bragard, Rimah Jaber, and Alliyah Gray, conducted a national survey to try to illuminate the reasons for parental vaccine resistance and hesitancy.
For the study COVID-19 Vaccine Hesitancy Among Parents of Children Under Five Years in the United States, Fisher, and her team collected data in April and May 2022, a month prior to the vaccine approval. They partnered with the survey aggregator Qualtics XM, and after receiving 1,337 responses to a call to participate, they settled on 411 English-speaking self-identified Hispanic and non-Hispanic Asian, Black, and white female guardians who were 21 or older and had children 1 to 4 years old. The results were published this month in the journal Vaccines.
They found that 31.3% of parents intended to vaccinate their child, 22.6% were unsure, and 46.2% intended not to vaccinate.
Their reasons were revealed in an open-ended section of questioning, where participants could go into greater depth about their concerns. One was the fact that the COVID BA.5 Omicron subvariant, which has become the dominant strain of the virus, is much more capable of infecting healthy people who have been vaccinated and boosted. That meant that some of the respondents had already had experience with infections, and those experiences did not lead them to automatically accept the need for vaccinations.
One mother, whose answer was classified in the study as “unsure,” wrote the following:
“The children had it, including my three-year-old, and the symptoms for him were very minor
to none. We actually had it twice and both times his symptoms were pretty minor. I also feel
like they should have some immunity against the virus now and getting shots every few months, without enough years gone by to see the side effects of the shot, just isn’t an option for us.”
Another, who was classified as “accepting,” still had safety concerns:
“I’m afraid because the words “emergency approval” kind of scares me especially when it comes to my children. I have a 3-year-old and an 8-month-old. Emergency makes it seem like it wasn’t tested as long as it needs to show proper results. However, most likely I will vaccinate my children”
Another concern that many parents also cited is the speed at which the vaccine was developed and approved. Relatedly, Fisher said it’s fair for parents to ask how many children have severe reactions to the vaccines, and in fact, the answer would allay their concerns.
“I read the data, and the data says that in fact, the vaccine has fewer side effects for young children than it does for adults. But you know, how many parents are going to read the research? The problem is that what’s effective about the vaccine is that those of us who are vaccinated are not hospitalized, and we don’t die when we get COVID. But that doesn’t necessarily get through to all parents,” Fisher said.
“Another thing is that a lot more parents have been vaccinated themselves, and have had these horrible, severe flu-like reactions [after vaccination]. They don’t want their young child to experience that.”
Compounding the problem is the fact that parents are not hearing these kinds of concerns addressed by authorities such as the Centers for Disease Control, Fisher said.
“You don’t hear on the ads that are going around that if you take the vaccine, you may get the new variant of COVID, but you won’t be hospitalized, and you won’t die,” she said.
“Nobody is addressing parents’ real concerns. They’re just saying, ‘Take the vaccine.’ And then parents are seeing that people who take the vaccine are getting COVID anyway.”
The need to recalibrate messaging on vaccines is taking on more importance, as recent statistics indicate that a year after vaccines became available to children between 5 and 11, fewer than 40 percent of that population has received two shots of the COVID vaccine, she said.
Research has found that children in that age range are more likely to suffer long-term side effects from COVID than from vaccines, and even though children who are infected generally suffer less severe symptoms than adults, they’re not immune. In rare instances, their symptoms can be very severe, and that shouldn’t be discounted by a parent who’s trying to decide whether to vaccinate or not.
But that can only be done if parents’ concerns are addressed, Fisher said.
“There is this very small percentage of parents that are resistant for resistance’s sake, whereas there are others who are just either misinformed or are highly concerned,” she said.
“What I’m hoping is that, because we did these narratives that allowed parents to speak in their own voice, it will alert pediatricians who are talking to parents to ask them what their concerns are, rather than just tell them, ‘The vaccine’s safe, your child should take it.’ That’s not going to work.”
]]>
The University has adopted the following COVID-19 protocols for the Fall semester:
Vaccinations
As of September 1, students, faculty, and staff are required to be fully up-to-date, as defined by the U.S. Centers for Disease Control and Prevention (CDC).
Students, faculty, and staff are responsible for updating their vaccine status in VitalCheck. Employees must send their proof of vaccination to VitalCheck at [email protected] and [email protected] (student proof of vaccination should only be uploaded into VitalCheck; see detailed instructions online). VitalCheck is linked to your Fordham ID card for ease of entry to campus. VitalCheck will also display proof of vaccination on your smartphone and may serve as the campus access card.
Individuals are eligible for the first booster 5 months after the final dose of the initial series; and may be eligible for a second booster 4 months after the first booster. The University will continue to consider medical and religious accommodations for individuals who request them.
The University will resume administering free COVID-19 vaccinations on campus beginning August 1.
Testing
The University will offer on-demand testing and testing for suspected exposure, and for students only, diagnostic testing, but will discontinue surveillance and return-to-campus testing in the Fall semester. (Employees who have COVID-19 symptoms should not come to campus, but should see their healthcare providers for diagnostic testing.)
The University will continue to require weekly testing for individuals with medical or religious vaccine accommodations, or who are not yet fully up-to-date with their vaccines.
Fordham recommends that everyone returning to campus for the Fall semester take a COVID-19 test (PCR or rapid antigen) prior to arrival on campus, especially individuals who are traveling from outside of the New York metropolitan area. Anyone who receives a positive test result should complete their isolation before coming to campus. In August, the University will share testing locations and times for the Fall semester.
VitalCheck Daily Screening
Fordham will discontinue required daily screenings on VitalCheck as of August 8. VitalCheck will continue to send a daily notification which can be used to report symptoms and access telehealth appointments (particularly for employees and graduate students), but users will not have to respond to the daily affirmation to continue campus access. The University will continue to use VitalCheck to manage vaccine, testing, and isolation requirements, and for integration with the ID card system for access to campus.
Masking
On campus, masks are recommended but not required in classrooms, labs, work settings, and public spaces for individuals fully up-to-date on vaccinations. (The CDC’s mask guidelines say that individuals may “wear a mask based on your personal preference, informed by your personal level of risk.”) All individuals may wear masks in any setting if they choose to do so. Faculty may require masks in classrooms and laboratory settings, if they believe the particular circumstances warrant such measures.
- Unvaccinated individuals with an exemption must still wear masks.
- Masks remain mandatory on Ram Vans and in University Health Service locations (offices, and testing and vaccination sites).
Contact Tracing and Isolation and Quarantine
The University is evaluating the current contact tracing protocols and will advise the community when more details are available.
There are no changes to the isolation and quarantine protocols: commuter and resident students who are able to travel to their homes will be directed to isolate or quarantine at their off-campus residences. Resident students who are unable to travel home will be isolated or quarantined in designated residence hall rooms.
Students and Employees who are up-to-date with their vaccinations do not have to quarantine upon exposure, but should monitor their health and be tested 5 days post exposure, or if symptoms appear. Anyone with vaccine accommodations is required to quarantine upon exposure. Employees who become ill on campus will be provided with guidance on isolation and quarantine requirements by Human Resources.
Visitor and Guest Policies
Beginning September 1, Fordham campuses will be open to non-Fordham visitors and guests, and to Fordham-sponsored external events. All visitors 6 months of age and older are expected to be up-to-date on vaccinations, as stated above, and the University will require proof of vaccination for entry to campus. More information and details on residence hall visitation and overnight guests will be provided soon by the Offices of Residential Life.
Employees with questions about Fordham’s COVID-19 policies should email vpforadministration@fordham.
As always, our policies and protocols are subject to change, based on conditions on and off campus, and any new federal, state, or local regulations. Thank you for your support and cooperation.
Marco Valera
Vice President for Administration & COVID-19 Coordinator












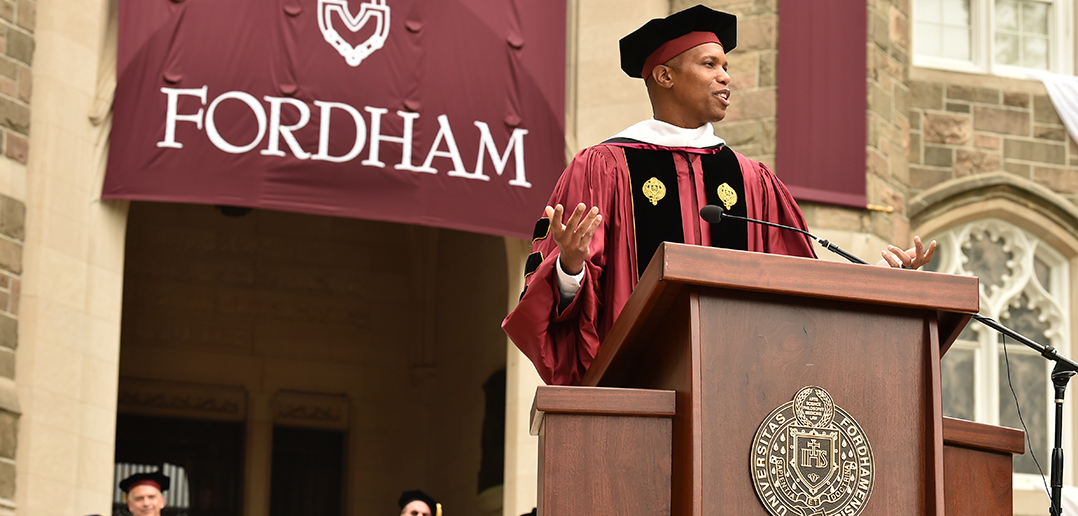


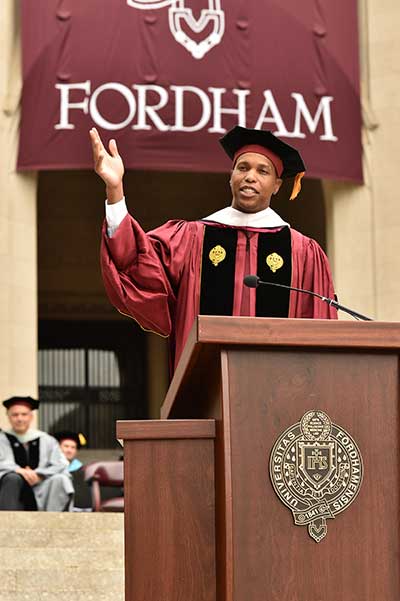
 Addressing 720 new master’s and doctoral graduates of the Gabelli School of Business on May 24, Mandell Crawley, chief human resources officer at Morgan Stanley, urged graduates to “be incredibly proud” of what they’d “accomplished during such an uncertain and challenging time.”
Addressing 720 new master’s and doctoral graduates of the Gabelli School of Business on May 24, Mandell Crawley, chief human resources officer at Morgan Stanley, urged graduates to “be incredibly proud” of what they’d “accomplished during such an uncertain and challenging time.”
Crawley, who received an honorary doctorate during the ceremony, recalled his own experiences in the executive MBA program at the Gabelli School during another fraught period: the Great Recession.
“I was in a cohort that represented many of the banking institutions engulfed by the crisis,” said Crawley, who earned his MBA in 2009 and has since risen to a series of high-profile senior leadership positions at Morgan Stanley, including chief marketing officer and head of the firm’s private wealth management business. “My classmates and I relied on each other and got through that experience together.”
Indeed, this idea of building community through a tough shared experience was a common theme at the ceremony, present in nearly every speech the audience heard. Throughout the afternoon, the graduates—including 20 military veterans who were also feted at a special Victory Bell-ringing ceremony on May 20—were cheered on by hundreds of friends, family, faculty, and members of the Fordham community who had gathered on Edwards Parade.
The Value of ‘Strategic Persistence’ and the Gabelli Network
Donna Rapaccioli, Ph.D., GABELLI ’83, dean of the Gabelli School, told graduates that their time together at the University helped them hone a capacity for what two-time Fordham graduate Caroline Dalhgren, director of global consumer insights at Tiffany & Co., calls “strategic persistence.”
“What does that mean? Caroline says it’s that Fordham graduates are ‘scrappy’ in the best possible way,” Rapaccioli said. “You do not expect that anything will ever be handed to you on a silver platter. Instead, you are go-getters. You are solution-finders. You know what you want—and you come up with exciting plans to get there.”
Rapaccioli described Dahlgren as an ideal member of the alumni community, someone who has helped hire many Fordham graduates in her role at Tiffany & Co. and who always says yes when Fordham students and alumni reach out to her for career advice. Rapaccioli encouraged graduates to do the same as active members of the Fordham alumni network—more than 200,000 people worldwide, including 40,000 Gabelli graduates, she said.
“When they contact you asking for career guidance, or when they email you asking for help in their job search, say yes,” she said. “As Caroline puts it, ‘We only will be successful in building this alumni network if we all say yes.’”
Graduate School in Turbulent Times
Addressing graduates at his final degree ceremony as president of Fordham, Joseph M. McShane, S.J., cited the challenges they encountered as they pursued their degrees: the COVID-19 pandemic and the financial instability it spurred, the country’s ongoing issues with race and inequality, and budding international political strife.
“My dear friends, let’s be honest: Your time in graduate school has not been an easy time,” he said. “You found yourselves in graduate business programs preparing to take on a world—and a global economy—at a time that both of them were seriously out of joint.”
He congratulated them on persevering, even as they “may have been a bit battered along the way,” and encouraged them to never forget the lessons they learned as Fordham students, namely how to be business professionals marked by competence, conscience, compassion “and deep commitment to the cause of the human family.”
A Heartfelt Tribute to Dean Rapaccioli

Father McShane also offered a special thank-you to Rapaccioli, who is stepping down at the end of June to return to teaching and research after a remarkable 15-year tenure as dean. He surprised her with a Magis Medal, making her the first-ever recipient of the award, established this year to honor longtime administrators who have strengthened the Fordham community “through their discerning wisdom, extraordinary leadership, and unstinting commitment to excellence in the service of others.”
“She has led the school with energy, vision, devotion, and love,” Father McShane said of Rapaccioli, who led the unification of the University’s undergraduate and graduate business schools in 2015, launched Gabelli’s first doctoral programs, and oversaw significant growth in enrollments and rises in rankings at the school. “In the process, she has transformed it and made it a leader not only in American business education, but a leader and trailblazer in international Jesuit business education. Therefore, we are all in her debt, a debt that is so great that I could never adequately thank her.”
Six faculty members were also recognized during the ceremony. Paul Kramer, GABELLI ’88, and Joseph Zirpolo, GABELLI ’98, each received the Dean’s Award for Faculty Excellence; Miguel Alzola and John Fortunato each received the Gladys and Henry Crown Award for Faculty Excellence; and Alex Markle and Iris Schneider each received the Stanley Fuchs Award, presented in memory of the former area chair of law and ethics who was a devoted teacher and student advocate.
A Framework for Fulfillment
In his remarks, Crawley, a native of Chicago’s West Side, spoke about his professional path. He has been working at Morgan Stanley for three decades, since he landed a work-study position with the company in high school.
“My journey was far from linear; it was quite circuitous,” he said. “I started out as a 17-year-old intern running errands for bond traders, earning a wage of $5 an hour, [and] worked my way across different parts of the Morgan Stanley ecosystem.”
He continued working on the firm’s municipal bond sales and trading desk in Chicago while attending Northeastern Illinois University at night, transferring to Morgan Stanley’s New York City headquarters once he’d earned his bachelor’s degree in economics. In 2004, he garnered his first management role, and in 2014, he was elevated to chief marketing officer, a position he held until taking over the company’s private wealth management business in 2017. He has been the firm’s global chief human resources officer since early last year.
Crawley shared two frameworks he uses to assess his professional progress—one to determine if it’s time to do something different, and one to determine what career he should be doing.
For the first, he told graduates to ask themselves four questions, suggesting that if the answer to any of them is ‘no,’ they may consider reevaluating their role: Am I learning? Am I growing? Am I having impact? Am I happy? Meanwhile, he said, graduates should ask themselves a second, broader set of questions: Am I interested in the work? Does it align with my core capabilities or superpower? Can I be useful?
Crawley used his love for basketball as an example of how interest doesn’t always align with capability. “I’m interested in the game. I’m a tall guy. Unfortunately, I wasn’t wired for it. The NBA won’t be reaching out to me anytime soon,” he joked. But he encouraged graduates to bring passion to their careers.
“The energy and enthusiasm you have right now? Do not lose it; let it drive you,” he said. “Channel it throughout what I know will be long and successful careers for all of you.”
Better Today Than Yesterday
The ceremony also featured two student speakers: Jason Gurtata, president of the Student Advisory Council and a graduate of the full-time MBA program, and Aaron Martins, who earned an M.S. in global finance.
Looking back to the beginning of his Gabelli journey, Gurtata remembered meeting his cohort for the first time—on Zoom.
He said that while they may not have fully understood what they were in for at the outset—”Did we have any idea of what it meant to immerse ourselves so deeply that all we did was dream about LinkedIn Premium features during our naps?”—he relished being on the other side and credited his Gabelli experiences for teaching him the “most important lesson”: Strive to be better today than yesterday.
As he and his classmates learned “not to chase dollars but to chase our dreams,” Gurtata said he not only gained a new family of Fordham Rams but he also learned the true meaning of success.
“Success is not a test score; it is not that job at a high-end bank, investment firm, or media company; it is not about your salary,” he said. “It is about who we are as individuals. We have learned to partake in business with a purpose, but I encourage each and every one of you to live your life with a purpose.”
Nowhere Near the End
Martins echoed the day’s theme of persevering through the pandemic’s “unchartered territory.”
“We showed that we will adapt and overcome whatever life will throw at us,” he said. “In difficult, uncharted territory we were still focused on our goals and aspirations, ready to keep moving forward.”
He stressed that while their Fordham education was concluding, the ceremony certainly wasn’t the end of the road.
“This may be the end of the chapter, but the book is far from over,” he said.
]]>Fordham University COVID-19 Guidelines on the web: fordham.edu/fordhamforward
Here are the five things you need to know about Fordham’s COVID-19 precautions, vaccinations, and University operations. As of this week, the University is suspending weekly Five Things emails: it will be published on an as-needed basis through the summer.
- On-Campus Cases: In the last 7 days, 67 members of the University community tested positive for COVID-19, as listed on the University dashboard.
- The COVID-19 Alert Level in New York City is MEDIUM: See the New York City Department of Health website which outlines the appropriate precautions for each alert level.
- Commencement Vaccination Requirements: The University requires all visitors to campus (ages 5 and older) to be fully vaccinated against COVID-19. One booster shot is required for all guests who are eligible. Please review the COVID-19 vaccination policy for more information.
- Fordham Vaccine Mandate: The University will continue to require all on-campus students, faculty, and staff to be fully up-to-date† on vaccinations for the 2022-2023 academic year. It may be necessary to require a second booster shot for eligible individuals beginning in September 2022.
- Testing and Vaccinations at Lincoln Center are now being administered in South Lounge.
†“Up-to-date” means the individual has received a full series of COVID-19 vaccines, and a booster shot, if eligible.
Every issue of Five Things is archived on our news site: news.fordham.edu/tag/five-
Marco Valera
Vice President for Administration & COVID-19 Coordinator